Acute Encephalitis Syndrome Reduction through Promotion of Environmental Sanitation and Safe Drinking Water Practices
- By
- Amal Kumar
- May-18-2020
Abstract: Water management and safe sanitation play an important role in controlling vector borne diseases in the tropical countries like India. Recent past year’s JE/AES outbreak in the Terai land of sub-Himalayan region of the Gangetic plains has been a issue of concern for the medical experts, environmentalists and policy makers. Thousands of victim children has lost their life due to JE/AES illness in India since year 2005. This outbreak of the Acute Encephalitis Syndrome (AES) is high during monsoon seasons every year and, the most affected age group with high rate of mortality and morbidity are the children 1-15 years aged. Directorate of National Vector Borne Disease Control Programme (NVBDCP), India has revised its guideline in the year 2009 to manage encephalitis as a result of entero-viral infections due to drinking of contaminated water. Though encephalitis illness can affect all people of any age group and any time of the year. Environmental sanitation and safe drinking water play a very crucial role in health of children. This research article is based on field study of 5 months and I collected the research data from the primary (community) as well as secondary (government) sources presents an overview of the water and sanitation related aspects impacting the lives of common people such as spread of vector borne diseases Japanese Encephalitis (JE)/Acute Encephalitis Syndrome (AES) in Lakhimpur Kheri district is one of the significant Terai land habitation being highly cultivated area in Uttar Prdaesh, India. The analysis include environmental-social changes, ecosystem-based adaptations, water-related common diseases and the corrective measures to prevent AES through improved sanitation, water management and community awareness about prevention of causative agents of AES. Collectively, this article recommends better planning of AES control globally, educate the community and strengthen the government health system technically and capacitate them to manage AES cases. The research study also aims to benefit health and water policy makers, researchers along with the betterment of the target community in Lakhimpur Kheri.
Introduction: Water management and environmental sanitation is closely linked with good health of the community living in urban as well as rural area of tropical and sub-tropical countries like India. Poor sanitation and unsafe drinking water is one the biggest cause of high child mortality rate in India (6). If someone lives in the poor environmental sanitation condition, consumes unhygienic food or drink contaminated water, it allows several types of pathogens enter into body and cause illness and sometimes serious infections like encephalitis, typhoid etc. can lead to death of a person. Encephalitis is an central nervous system disease marked by the acute on set of high grade fever and change in the mental status with or without new onset of seizers in patients especially children below 15 years age are at high risk of getting AES illness (1),(3).
Acute Encephalitis Syndrome (AES): (WHO Definition) A case with acute febrile illness and change in mental status (such as confusion, disorientation, inability to talk, coma) with or without new onset seizures, excluding simple febrile seizures. There exists several etiologies for AES but Government of Uttar Pradesh has instructed to conduct 5 mandatory test for each AES case i.e. Japanese Encephalitis, Scrub Typhus, Dengue, Chikanguniya and Malaria (3),(5). These all 5 types of etiology are compulsory in each symptomatic AES suspect case management and, are linked with environmental sanitation and water management practices.
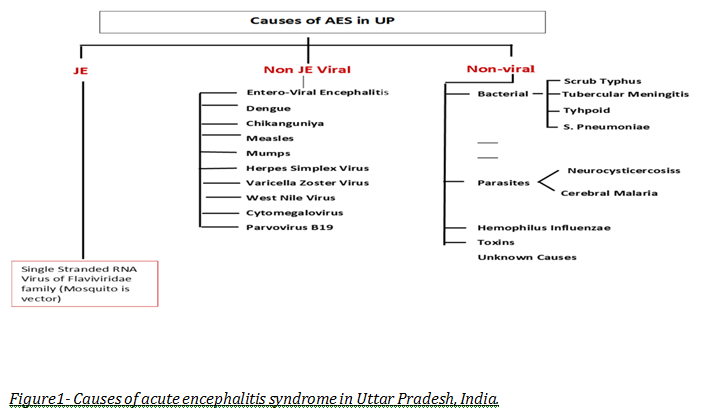
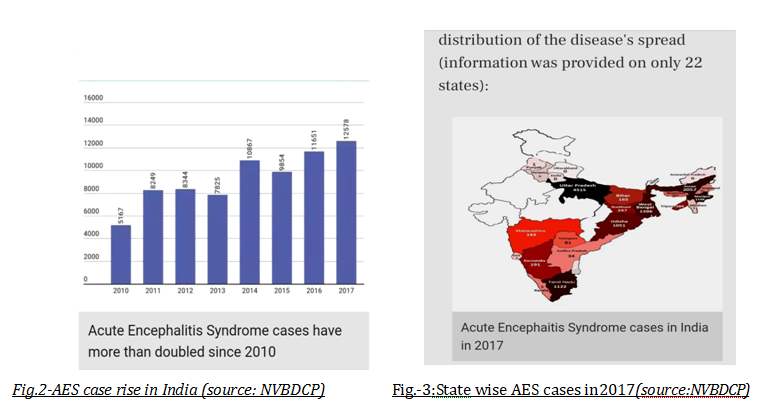
The rising number of AES cases in the country is mainly due to rapid and unplanned urbanization, poorly developed towns, and villages are void of safe sanitation, drinking water facility and behaviour change communication to promote good sanitation practices. According to NVBDCP a total 12,578 cases were affected by AES in 2017, a rise over 243 percent since 2010 AES outbreak of encephalitis in India. It is evident that large proportion of AES cases in Uttar Pradesh are caused by a bacterium called scrub typhus (5),(7) or bush typhus followed by Japanese Encephalitis virus. This, in turn, was linked to environment and living conditions around people tested positive with AES. Uttar Pradesh carried the largest AES burden in India for a long time possibly due to various reasons; socio-political, environmental and economic conditions. (10,11).
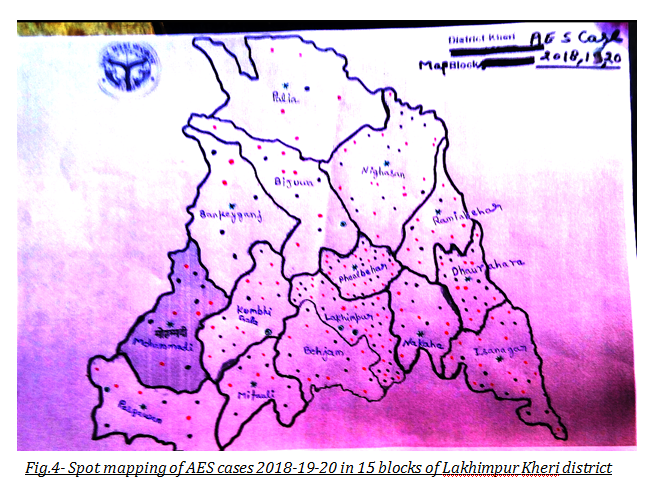
Tackling AES through Community led Water Management and Sanitation in Kheri, Uttar Pradesh: Lakhimpur Kheri is one of the largest Terai land District in state of Uttar Pradesh. It consists of 15 Blocks and comes under Lucknow division and, often in news due to flood conditions and JE/AES outbreak in monsoon seasons(9),(10),(11). It is one of the highly cultivated zone because of alluvial soil texture and irrigation facilities mediums are available e.g. rivers, canals, wetlands and motor pumps etc. The agricultural crops in practice are sugar cane, paddy, wheat, pulses, mustard and vegetables. Agriculture being primary occupation of the people in the region(8). The poor women(4) are often working in the farm field along with their children having much chances of exposure to vectors of the AES disease like chiggers are source of fatal scrub typhus lives inside the ears of rodents (17) and found on bushes(7). Water birds, pigs are host of JE virus, moreover paddy field is breeding ground for the mosquitoes Culex family (mainly Culex tritaeniorhynchus) and, if they bites on human body may cause JE illness. The poorest community residing in rural (2), peri-urban setting are more prone to getting AES as they hardly practice the safe hand washing with soap before cooking and eating food and, are not aware of significance of getting drinking water from a safe source like India marka-2 type hand pump, piped water supply and/or store it properly for later use (5). Therefore they drink contaminated water unknowingly and are habitual to live in a poor sanitation condition. Children and women are the most affected group lacking the safe sanitation, especially in monsoon seasons and/or flood conditions in terai belt of Lakhimpur Kheri (12),(13)(14). The AES case rise is high during July to November every year mostly in the flood affected Blocks. Table-1 and figure-4 is showing the spot mapping of AES cases block wise in the district. Those blocks are repeatedly facing the monsoon flood crisis every year, same time they have had the higher number AES cases as well(15),(16). Out of the total 15 blocks in the Kheri district the AES cluster found in most flood affected blocks i.e Phoolbehar, Ramiabehar, Isanagar, Bijuwa, Dhaurahara and Lakhimpur. In the figure-4, Red star is indicating the district hospital, green star indicating the blocks with encephalitis treatment centre, red points are marked for AES cases in year 2018, black points are marked for AES cases in year 2019, green points are marked for AES cases in year 2020. After visiting the each household with AES case in year 2018, 2019 and 2020, It was observed that the affected community is residing in locality of the poor environmental sanitation conditions and, are void of access to safe drinking water. It is evident through analysis of AES case line-list of integrated disease surveillance programme unit (IDSP) Kheri for past three years that 80 percent AES cases are directly linked with the water management and sanitation(18),(19).
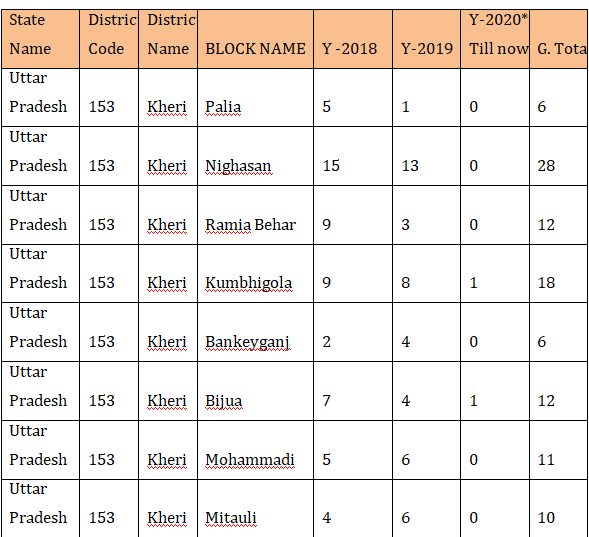
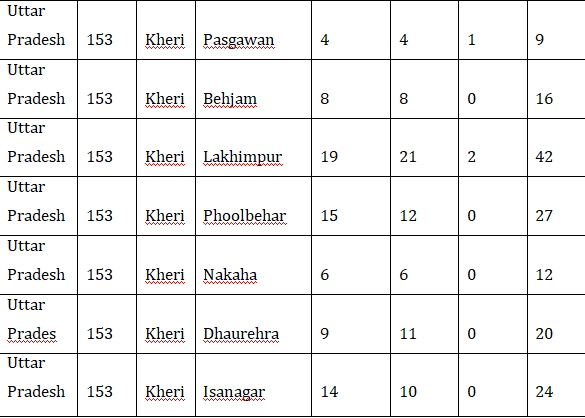
Table-1 : Block wise AES cases in 2018-19-2020 Lakhimpur Kheri
Some corrective measures have been taken by the government of Uttar Pradesh to improve sanitation by the involvement of municipal body in the urban areas and Panchayati Raj Institutions in the rural areas. There require more efforts to revise the state water policy and sanitation infrastructure development in order to achieve the SDG-6. Development actors working on water and sanitation can play important role to intervene in-between the target community to engage them and help to create an aware society with the help of communication behavior change strategy. In order to increase the utility of the agricultural by-product and waste management in terms income generation for the poorest community, there must be provision of public private sector partnership with efforts of the state government and ensure the technology transfer between the farmers group on appropriate subsidy as they could adapt scientific farming. It shall be beneficial for the environment (26) as well increase the income of small farmers including women farmers. Strengthen the government system to address the water and sanitation issues in the most affected area primarily and later on cover all blocks to reduce AES cases through improved water management and good sanitation. Women play productive as well as reproductive role in the society, therefore they must be given utmost importance and have access to water and sanitation facility. Frontline workers (FLWs) like ASHA, Aganwadi workers, ANM’s role is crucial to educate the rural and urban women about the management of drinking water, personal hygiene and sanitation, and, routine immunization including JE vaccination to avoid encephalitis due to Japanese Encephalitis Virus. Capacity building of health workers and FLWs as they could educate the women of the poorest community, chlorinated drinking water, upgraded sanitation, hand washing with soap, Infant and young child feeding practices to reduce malnutrition and improve immunity of the children and family at large against water/vector borne diseases.
Programme for Appropriate technology in Health (PATH) organization is implementing AES project in 11 most affected districts of Uttar Pradesh. At Lakhimpur Kheri District PATH organization has introduced Encephalitis Treatment Model (ETCs) in 11 high risks blocks and main objective of ETCs to decrease the morbidity and mortality of AES cases through ensuring prompt treatment, early oxygenation and referral. The project is providing technical support to the government of Uttar Pradesh to establish ETCs at government hospitals for the treatment of AES case, and sensitize the community by involvement of FLWs about preventive measures against AES illness(20)(21). It shall be given utmost importance to protect the community from exposure to vectors of AES disease in a holistic way by engaging the multi-stakeholders like health, education, agriculture, animal husbandry, panchayat raj institutions, rural development, urban development and municipality, and, public health engineering department (PHED). These allied departments shall act in coordination under supervision of the district magistrate and work to control the vectors of AES diseases, ensure early referral of cases to nearest ETC, oxygenation and prompt treatment. Other than this, Integrated activities to prevent AES (28) are includes bush cutting, fogging and anti larval activity at the society places, chlorination of drinking water, India Marka-2 type hand pump installation in between the poorest community not having access to piped water supply, demonstration and training of compost making for the small farmers and other sustainable income generation activities for the women group along with health education programme for the children(27), youth and behaviour change communication in-between the target community. Public private sector partnerships, CBOs, NGOs, Educational Institutions, PRIs and local volunteers can play important role in implementation of above said activities and ensure the sustainability of AES reduction programme from Terai land in Uttar Pradesh and other regions worldwide (24),(25).
Conclusion: This article is based on field research study and I report for the first time that number of AES cluster through spot mapping is high in the blocks where flood conditions(22),(23) occurred every year causing water logging problem, contamination of drinking water and adversely affect the environmental sanitation. It is necessary to improve the water management practices amongst the community through an sustainable model of empowerment on environmental sanitation. Such kind of environmental sanitation intervention shall be community led and, also involve the development actors in same field, public private sector partnerships for the agricultural waste management and employment generation, capacitate allied government departments and fix their liability at policy level to meet the expected outcome (29). In order educate, aware and engage the women group and turn them as activists to reduce AES through improved environmental sanitation and water management. This way an aware community is adapt to good sanitation practices like hand washing with soap, manage agricultural waste and livestock waste into compost making, manage drinking water and grey water to prevent vector borne diseases as well as protection against COVID-19 pandemic.
References:
1. Rahman M, Wojtyniak B, Rahaman MM, Aziz KM. Impact of environmental sanitation and crowding on infant mortality in rural Bangladesh. The Lancet. 1985 Jul 6;326(8445):28-30.
2. Reddy, T.S. and Reddy, V.P., 2020. Information Sources Sought by Rural Community of Select Gram Panchayats of Atmakur Mandal of SPSR Nellore District, Andhra Pradesh. Pearl: A Journal of Library and Information Science, 14(1), pp.84-101.
3. Kumari, R. and Joshi, P.L., 2012. A review of Japanese encephalitis in Uttar Pradesh, India. WHO South-East Asia Journal of Public Health, 1(4), pp.374-395.
4. Kaur, L., Kaur, S., & Sharma, P. (2019). Information-Seeking Behaviour of Women Regarding Household Health and Hygiene Practices. Current Journal of Applied Science and Technology, 1-8.
5. Thangaraj, Jeromie Wesley Vivian, Mahima Mittal, Valsan Philip Verghese, CP Girish Kumar, Winsley Rose, R. Sabarinathan, Ashok Kumar Pandey, Nivedita Gupta, and Manoj Murhekar. "Scrub typhus as an etiology of acute febrile illness in Gorakhpur, Uttar Pradesh, India, 2016." The American journal of tropical medicine and hygiene 97, no. 5 (2017): 1313-1315.
6. Srikanth, R. "Challenges of sustainable water quality management in rural India." Current Science (2009): 317-325.
7. Mittal, Mahima, Jeromie Wesley Vivian Thangaraj, Winsley Rose, Valsan Philip Verghese, CP Girish Kumar, Mahim Mittal, R. Sabarinathan, Vijay Bondre, Nivedita Gupta, and Manoj V. Murhekar. "Scrub typhus as a cause of acute encephalitis syndrome, Gorakhpur, Uttar Pradesh, India." Emerging infectious diseases 23, no. 8 (2017): 1414.
8. Namara, R.E., Hanjra, M.A., Castillo, G.E., Ravnborg, H.M., Smith, L. and Van Koppen, B., 2010. Agricultural water management and poverty linkages. Agricultural water management, 97(4), pp.520-527.
9. Anukumar, B., Gajanan N. Sapkal, Babasheb V. Tandale, R. Balasubramanian, and Daya Gangale. "West Nile encephalitis outbreak in Kerala, India, 2011." Journal of Clinical Virology 61, no. 1 (2014): 152-155.
10. Dinesh, D.S., Pandey, K., Das, V.N.R., Topno, R.K., Kesari, S., Kumar, V., Ranjan, A., Sinha, P.K. and Das, P., 2013. Possible factors causing acute encephalitis syndrome outbreak in Bihar, India. Int J Curr Microbiol App Sci, 2(12), pp.531-538.
11. Bandyopadhyay, B., Chakraborty, D., Ghosh, S., Mishra, R. and Rahman, M., 2015. Epidemiological investigation of an outbreak of acute encephalitis syndrome (AES) in Malda district of West Bengal, India. Clin Microbial, 4, pp.181-187.
12. Fisher, J., 2006. For her it's the big issue: putting women at the centre of water supply, sanitation and hygiene. Water, Sanitation and Hygiene Evidence Report.
13. Singh, N., 2006. The changing role of women in water management: Myths and realities.
14. De Sousa, Aline Andrade, Renata Reis, João Bento-Torres, Nonata Trévia, Nara Alves de Almeida Lins, Aline Passos, Zaire Santos et al. "Influence of enriched environment on viral encephalitis outcomes: behavioral and neuropathological changes in albino Swiss mice." PloS one 6, no. 1 (2011).
15. Pires, Diego A., and Raquel M. Gleiser. "Mosquito fauna inhabiting water bodies in the urban environment of Córdoba city, Argentina, following a St. Louis encephalitis outbreak." Journal of Vector Ecology 35, no. 2 (2010): 401-409.
16. Misra, U.K., Kalita, J., Goel, D. and Mathur, A., 2003. Clinical, radiological and neurophysiological spectrum of JEV encephalitis and other non-specific encephalitis during post-monsoon period in India.
17. Peden, D., 1998. Agroecosystem management for improved human health: applying principles of integrated pest management to people.
18. Tyagi, B. K. "Advancement in the control of neglected tropical vector-borne diseases in the 21st Century, with special reference to India."
19. Mallanna, C. and Kolhapure, D.A., 2020. Drinking Water Supply Status in Habitaions with Population Coverage-A Geographical Study. RESEARCH JOURNEY, p.153.
20. Minkler, M., Vásquez, V.B., Tajik, M. and Petersen, D., 2008. Promoting environmental justice through community-based participatory research: the role of community and partnership capacity. Health Education & Behavior, 35(1), pp.119-137.
21. Dutta, K. and Basu, A., 2017. Overview on Japanese Encephalitis in South and Southeast Asia. In Neglected Tropical Diseases-South Asia (pp. 277-327). Springer, Cham.
22. Tapsell, Sue M., Edmund C. Penning-Rowsell, Sylvia M. Tunstall, and Thomas L. Wilson. "Vulnerability to flooding: health and social dimensions." Philosophical transactions of the royal society of London. Series A: Mathematical, Physical and Engineering Sciences 360, no. 1796 (2002): 1511-1525.
23. Alderman, K., Turner, L.R. and Tong, S., 2012. Floods and human health: a systematic review. Environment international, 47, pp.37-47.
24. Vanlerberghe, V.E.E.R.L.E., Toledo, M.E., Rodriguez, M., Gomez, D., Baly, A., Benitez, J.R. and Van Der Stuyft, P., 2009. Community involvement in dengue vector control: cluster randomised trial. Bmj, 338, p.b1959.
25. Lloyd, L.S., Winch, P., Ortega-Canto, J. and Kendall, C., 1994. The design of a community-based health education intervention for the control of Aedes aegypti. The American journal of tropical medicine and hygiene, 50(4), pp.401-411.
26. Ault, S.K., 1994. Environmental management: a re-emerging vector control strategy. The American journal of tropical medicine and hygiene, 50(6_Suppl), pp.35-49.
27. Deepthi, R., Naresh Kumar, S.J., Prasanna Kamath, B.T. and Rajeshwari, H., 2014. Participatory school health education on vector-borne diseases: engaging children as change agents. International Journal of Health Promotion and Education, 52(2), pp.68-77.
28. World Health Organization, 2004. Global strategic framework for integrated vector management (No. WHO/CDS/CPE/PVC/2004.10). World Health Organization.
29. Breilh J, Parkes MW, Bienen L, Hsu LN, McDonald M, Patz JA, Rosenthal JP, Sahani M, Sleigh A, Waltner-Toews D, Yassi A. All Hands on Deck: Trans disciplinary Approaches to Emerging Infectious Disease.
Acknowledgements: I’m thankful to national vector borne disease control programme (NVBDCP), government of Uttar Pradesh and PATH organization for their great efforts and new initiatives to reduce the number of AES cases through integrated preventive measures and establishment of encephalitis treatment centres in the 18 high risk districts of Uttar Pradesh. I am also thankful to IDSP unit Kheri for their support in research work related to acute encephalitis syndrome.
Author Information:
SEMRAI, Gola Gokarannath, Lakhimpur Kheri, Uttar Pradesh, India ( 262802).
Email: mukesh.envo@gmail.com
Contact No: +91 979-598-3487
Date of Birth: 15/07/1978
LinkedIn account: https://www.linkedin.com/in/mukesh-kumar-shukla-4325287a
Biography:
Mukesh Shukla has his expertise in child health, nutrition, WASH and biodiversity conservation. Currently working as District Coordinator in Program for Appropriate Technology in Health (PATH) at Lakhimpur Kheri, U.P. India. Earlier he worked as Nutrition and WASH Expert for Nutrition Smart Village project in Chhatarpur, M.P. and worked as Project Officer in Centre for Environment Education, India for river biodiversity conservation education programme. Recently he structured an independent project on the topic of community led water management and sanitation, health education programme.